Controlled substances are drugs regulated by the government due to their potential for abuse or dependence. In Colorado, these substances are classified into specific schedules, each with its own set of rules and restrictions.
Understanding Colorado controlled substances is essential for healthcare providers, patients, and anyone navigating the state’s drug laws. This guide provides a comprehensive overview of Colorado’s controlled substances schedules, regulations, and their implications for individuals and communities.
What are Controlled Substances?
Controlled substances are drugs or chemicals whose manufacture, possession, and use are regulated by the government. These substances are categorized based on their potential for abuse, medical value, and safety.
The federal Controlled Substances Act (CSA) establishes the framework for drug regulation, but states like Colorado also enforce their own laws to address local needs.

Colorado Controlled Substances Act
Colorado’s Controlled Substances Act aligns with federal guidelines but includes state-specific provisions to address local challenges. The act aims to:
- Prevent the abuse of prescription and illicit drugs.
- Ensure the safe use of medications for legitimate medical purposes.
- Regulate the distribution and dispensing of controlled substances.
By categorizing drugs into schedules, Colorado’s law provides a clear framework for enforcement and compliance.
Colorado Drug Schedules
Colorado classifies controlled substances into five schedules based on their potential for abuse and accepted medical use. Here’s a breakdown of each schedule:
Schedule I:
- Characteristics: High potential for abuse, no accepted medical use.
- Examples: Heroin, LSD, ecstasy, and marijuana (under federal law; Colorado has separate regulations for marijuana).
Schedule II:
- Characteristics: High potential for abuse, accepted medical use with severe restrictions.
- Examples: Oxycodone, fentanyl, Adderall, and methamphetamine.
Schedule III:
- Characteristics: Moderate potential for abuse, accepted medical use.
- Examples: Anabolic steroids, ketamine, and certain painkillers like codeine with aspirin.
Schedule IV:
- Characteristics: Low potential for abuse, accepted medical use.
- Examples: Xanax, Valium, Ambien, and Tramadol.
Schedule V:
- Characteristics: Lowest potential for abuse, accepted medical use.
- Examples: Cough syrups with codeine and certain antidiarrheal medications.

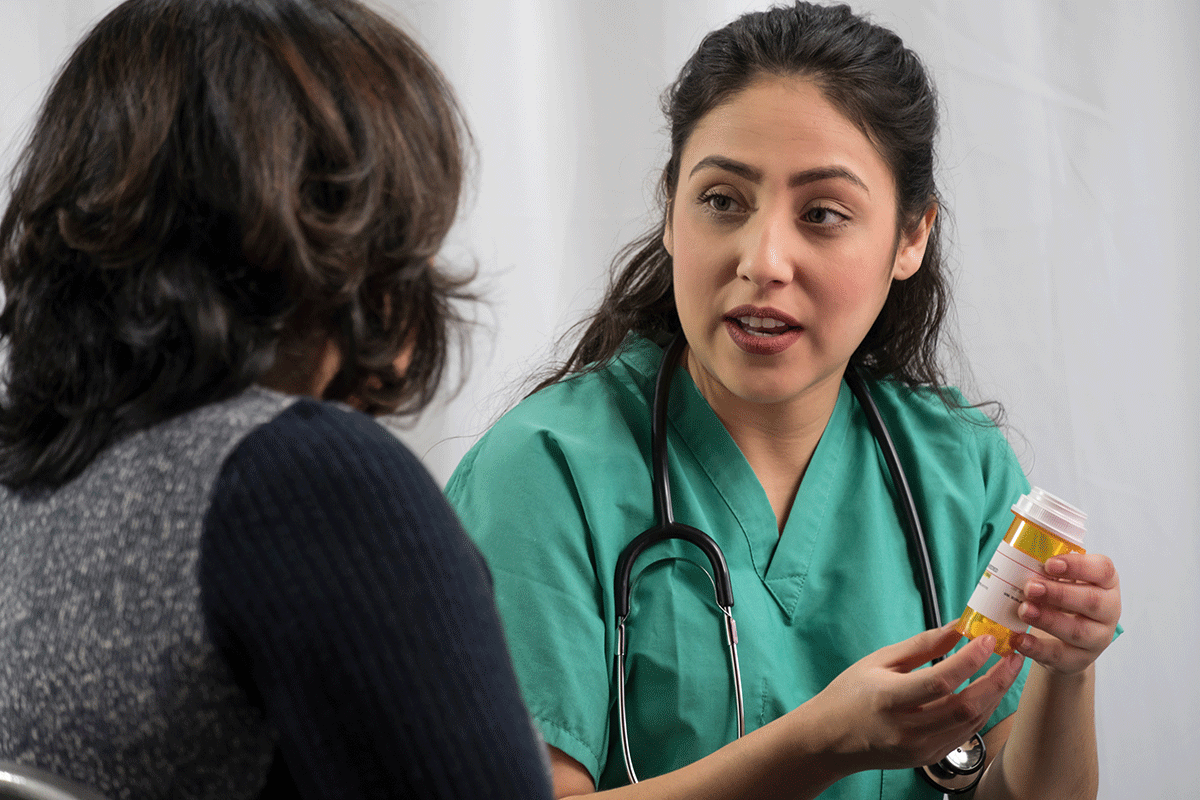
Prescription Drug Regulations in Colorado
Colorado has specific rules for prescribing and dispensing controlled substances to prevent misuse and ensure patient safety. Key regulations include:
- Prescription Monitoring Program (PMP):
- Healthcare providers must check the PMP before prescribing opioids or other controlled substances to identify potential misuse.
- Opioid Prescription Limits:
- Colorado limits the duration and dosage of opioid prescriptions for acute pain to reduce the risk of addiction.
- Healthcare Provider Requirements:
- Providers must follow strict guidelines when prescribing controlled substances, including documenting medical necessity and monitoring patient use.
- Pharmacist Responsibilities:
- Pharmacists are required to verify prescriptions and report suspicious activity to authorities.
Penalties for Violating Colorado Controlled Substance Laws
Violating Colorado’s controlled substance laws can result in serious legal consequences.
Penalties vary depending on the type and quantity of the substance, as well as the nature of the offense (e.g., possession, distribution, or manufacturing).
- Possession:
- Possessing a controlled substance without a valid prescription can lead to misdemeanor or felony charges, depending on the drug’s schedule and quantity.
- Distribution or Trafficking:
- Selling or distributing controlled substances is a felony offense, with penalties ranging from fines to lengthy prison sentences.
- Manufacturing:
- Producing controlled substances, such as methamphetamine or synthetic drugs, is a serious felony with severe penalties.

How CMAR Supports Compliance and Recovery in Colorado
While CMAR does not enforce laws, we provide education and support for individuals navigating Colorado controlled substances regulations.
Our outpatient detox and recovery programs help individuals struggling with substance use disorders, including those involving controlled substances. By offering resources and personalized care, we aim to support recovery and promote compliance with state laws.
FAQs About Colorado Controlled Substances
Colorado’s drug schedules align with federal guidelines but may include additional state-specific regulations.
Yes, Colorado allows the use of medical marijuana for qualifying patients, but it remains a Schedule I substance under federal law.
Penalties vary based on the drug’s schedule and quantity but can include fines, probation, or imprisonment.
Colorado limits opioid prescriptions for acute pain and requires healthcare providers to use the Prescription Monitoring Program (PMP).
The Colorado Department of Regulatory Agencies (DORA) provides a comprehensive list of controlled substances under state law.
Conclusion: Staying Informed About Colorado Controlled Substances
Understanding Colorado controlled substances is essential for compliance, safety, and recovery. Whether you’re a healthcare provider, patient, or concerned individual, staying informed about drug schedules and regulations can help prevent misuse and support recovery.
At CMAR in Denver, Colorado, we’re committed to providing resources and support for individuals navigating these complex laws.